🔬 Most Key Monoclonal Antibody Treatments Against OMICRON Are Now Ineffective - New Studies Show
On 11/26/21 the World Health Organization classified a new SARS-CoV-2 variant named B.1.1.529, more popularly known as OMICRON, and certified it as a novel VOC (variant of concern)1. Within days, questions regarding current vaccine and therapeutic efficacy against the newly discovered progeny surfaced. Simultaneously, genetic sequencing out of Botswana revealed a multitude of genomic changes in the new variant which further sparked international debate over possible immune escape, waning protection from primary series of COVID-19 vaccinations, and the possibility of reduced monoclonal antibody efficacy. Soon after, studies began to surface showing decreased effectiveness of current monoclonal antibody treatments against omicron.
In this publication you will learn 4 things:
Omicrons specific genomic changes and their importance
Why omicron is overpowering most key monoclonal antibodies
Important data from new monoclonal antibody studies
What all this means for you and your family
🔬Omicron’s mutations and deletions - how they’re important
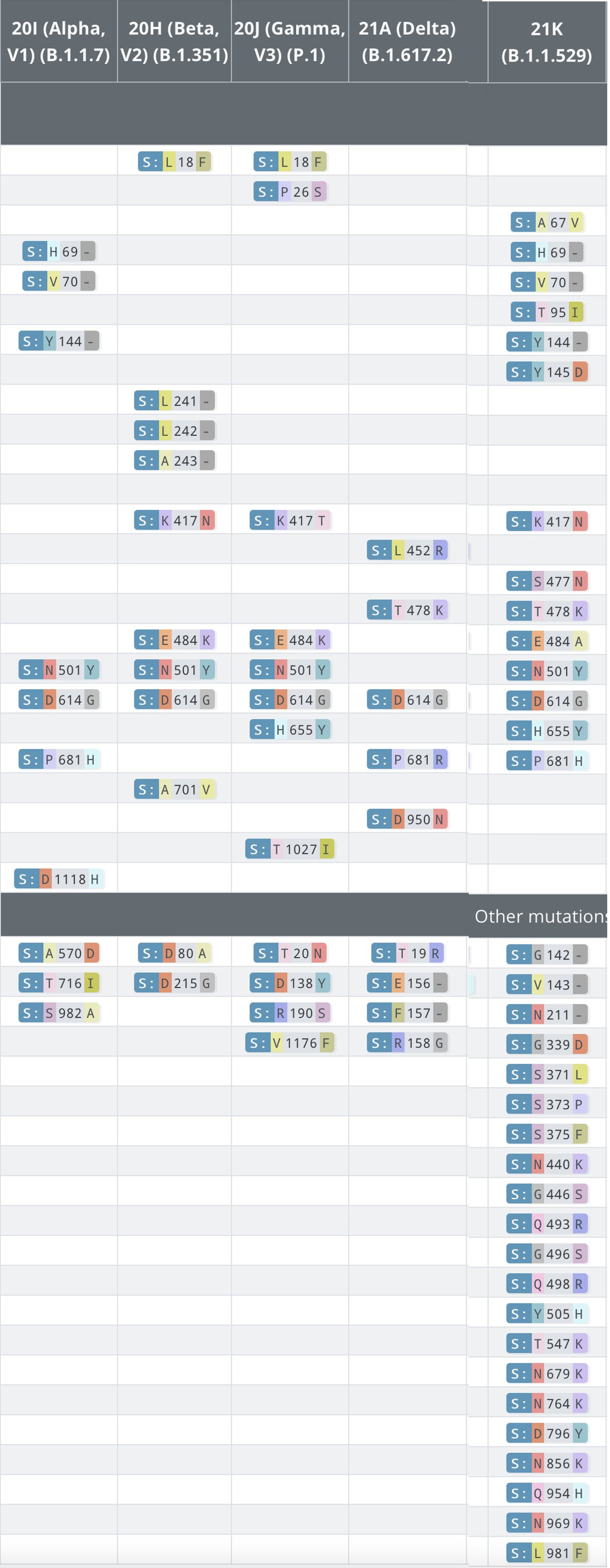
Initial sequencing out of Botswana revealed vast mutations and deletions in omicrons genetic code. To be precise, about 50 mutations, and 6 deletions were recorded. Essentially, those amendments in the variants code affect how the virus will act in the human body. Be that as it may, in order to understand how the changes are important, you first need to learn WHERE THE KEY CHANGE LIE. That said, KEY MUTATIONS in omicron and explanations of said alterations will be listed in bullet points below with supporting image FIG. 1. Moreover, A CHART OF ALL MUTATIONS can be seen after the first image in FIG. 2:
🔔 KEY MUTATIONS:
30 mutations found in spike protein
15 of the 30 spike mutations were in the RBD (receptor binding domain)
Together mutations ➡️ 1.) K417N, 2.) S477N, 3.)Q498R, 4.)N501Y with combined actions from these singular mutations ➡️ Q339D, S371L, S373P, S375F work as a team that enable omicron to 1.) evade antibodies, while also 2.) prevent antibodies from proficiently attaching to the mutated spike protein on the virus (SEE FIG. 1 #1)
Near the furin cleavage site located on the spike protein are more changes. Specifically, amended combinations of amino acids at ➡️ H655Y, N679K, and P681H, increase transmissibility of the new variant2. That is because furin, a protease from the human body that initiates the attachment process of the virus to host ACE2 receptor, doesn’t recognize the mutations at the furin cleavage site (H655Y, N679K, P681H) that it was previously trained to avoid as a result of previous exposure, or to some degree after vaccination3. As a result, furin cleaves, or makes cuts at the newly mutated cleavage site. Thus, viral infection of host cell ensues with less resistance (SEE FIG. 1 #4)4
Deletions at ➡️ 69, 70, 143, 144, 145, and 211 change the way the body recognizes and reacts to certain areas of the virus (SEE FIG. 1)5
Deletions at positions ➡️ L105, S106, and G107 inside of NSP6 (non-structural protein 6) help omicron avoid the immune system as said deletions substantially inhibit the host type 1 IFN response- a cytokine mediated response and immune detection system (SEE FIG. 1)6
🔔 LIST OF ALL MUTATIONS
A full chart denoting all 50 mutations can be seen in 📸 FIG. 2 down the column that say 21k B.1.1.529
🤔 SO HOW IS ALL OF THAT INFORMATION IMPORTANT?
Generally speaking, all aforementioned information is evidence of how the omicron variant avoids and impedes the immune response. In other words, the changes aka mutations in the genetic code make it more difficult for our bodies to recognize, kill, or fight the virus. To be precise, the key mutations above explain the most impactful changes, relative to the human body. But, how exactly is omicron evading monoclonal antibodies (keep reading to find out)?
📸 FIG. 1
📸 FIG. 2
🦠Why omicron is overpowering most key monoclonal antibodies
In order to understand how omicron outcompetes many current monoclonal or even polyclonal antibody treatments, you must first understand their mechanisms of action. The following paragraphs will explain 2 things. First, the history of monoclonal antibodies. Second, their current mechanisms of action (aka how they work) against SARS-CoV-2.
To begin, some history. In 1776, Dr. Edward Jenner was the first person to indirectly use antibody therapy to generate immunity against smallpox. Simply put, he inoculated non-exposed individuals with fluid from smallpox legions which later generated protection against the disease. Fast forward to 1975, Drs Kohler and Milstein engineered a way to duplicate antibodies with the highest affinity for their target antigens in large batches. After that, those large batches were broken down into smaller batches and administered to people during the onset of specific diseases to neutralize pathogenic molecules. In other words, in the lab, antibodies that destroyed their target with the highest proficiency were isolated and cloned then given to patients to combat disease in the early phases so the patients wouldn’t get as sick. Unfortunately, many people became ill from the treatment so adjustments were made to ameliorate the severity of reactions experienced by recipients. Let’s move ahead to current day. Monoclonal antibodies against SARS-CoV-2 are derived from either human convalescent plasma or humanized mice after being exposed to SARS-CoV-2 antigens or virus (FIG. 3). Said exposure results in robust antibody production which is then extracted from either host mice or human serum (blood). Following that, the serum is tested in the lab against SARS-CoV-2 like antigens to see which antibodies react most efficiently. The winners are then separated, duplicated, and given as treatment to others in need.
To bring things to a microscopic level, mechanisms of action will now be explained. To clarify, mechanism of action is how a drug, vaccine, or therapeutic produces an effect. Know this to start. There are 5 antibody classes. They are named IgM, IgD, IgG, IgE, and IgA. Moreover, all EUA approved monoclonal antibodies for COVID-19 are from the IgG class and this is how they work. First, the antibodies are infused/injected into the ill individual and find their way to the target antigen on the SARS-CoV-2 infected cell/molecule. Finally, they attach to the invader and then a conformational change (physical change) occurs in the fraction constant of the antibody, thus beginning compliment activation7. To put it another way, when the antibody finds the antigen, it attaches, then signals an immune cascade where all sorts of cells come over to fight off the intruder.
🤔 SO HOW IS OMICRON OVERPOWERING MOST MONOCLONAL ANTIBODIES?
A general explanation will be given first. Then second, the following paragraphs will detail specifics.
Number one, a general explanation. Monoclonal antibodies are specifically engineered to target particular antigens. Unfortunately, if the virus mutates, or changes, the monoclonal antibodies will be targeting an area of the invader that no longer exists. The result, the antibodies will not locate their target and the resulting evasion will increase the rate of infection and likelihood of symptomatic disease. The biggest problem with omicron is that there are 15 mutations on the receptor binding domain. Just so it’s clear, the receptor binding domain is what the virus uses to directly attach to human ACE2 receptors, then subsequently infect human cells. Well, current monoclonal antibodies target the pre-mutated receptor binding domain and regrettably don’t see the newly mutated receptor binding domain in the virus which leads to an inability of monoclonal antibodies to neutralize omicron. That means, the monoclonal antibodies pass right by omicron because they can’t appropriately identify it as a threat.
Number two, the specifics. To go into detail, there are currently 4 popular monoclonal antibody treatments, which are either singular antibodies or combination cocktails that have received EUA (emergency use authorization) in the USA: bamlanivimab plus etesevimab (Eli Lilly), casirivimab plus imdevimab (Regeneron), sotrovimab, and tixagevimab co-packaged with cilgavimab (AstraZeneca)8. They are advised for non-hospitalized individuals with mild to moderate symptoms. The most important part about monoclonal antibodies from Eli Lilly (bamlanivimab plus etesevimab), Regeneron (casirivimab plus imdevimab), AstraZeneca tixagevimab co-packaged with cilgavimab, and Sotrovimab is that they target the SARS-CoV-2 receptor binding domain amino acids in 2 conformational stages- open and closed9 (SEE FIG. 4). To explain, a conformational change in this case is a physical change that allows spike protein from the virus to appear different to monoclonal antibodies and the immune system. Said differently, if monoclonal antibodies and the immune system were looking for an unchanging structure, it would make the job much easier. However, sneaky conformational changes in the viruses spike protein make it very difficult to detect, and that hastens viral infection of human cells. That is why COVID-19 is so deleterious in general. Add to that RBD (receptor binding domain) mutations, and omicron becomes nearly unrecognizable to monoclonal antibodies.
So thats the bad news. Omicron has 15 mutations in the open and closed RBD (receptor binding domain) positions, so the monoclonals are not detecting this new variant proficiently. Yet, new studies show there is one monoclonal antibody still demonstrating decent efficacy against omicron. Keep scrolling to read about the new data 👇🏻.
📸 FIG. 3
📸 FIG. 4
📚 The studies
Virtually all new pertinent data from recent preprints are showing that most popular monoclonal antibodies, and vaccine induced antibodies, are nearly powerless against the omicron variant during testing (1st and most recent study here, 2nd study here, 3rd study here, 4th study here). The strongest correlation is seen in this study here.
Let’s start with a disclaimer. Although the aforementioned literature has not been peer reviewed, it will be soon. Even so, all good data needs to be considered. Moreover, many companies already concede their monoclonal antibody products are less effective against omicron so all available data needs to be reviewed. Moving on.
As a summary of all data presented in the studies listed above, it is true in all cases that when placed against omicron, the power of plasma neutralizing activity was significantly diminished. That means, when omicron was isolated then challenged, it outcompeted 1.) antibodies from sera of vaccinated individuals, 2.) most monoclonals, and 3.) antibodies from previously infected people. Interestingly, sotrovimab, VIR-7832, and combination COV2-2131+2196, stood up to the variant very well. To be exact, there was only a 2-fold reduction in neutralizing antibody efficiency against omicron with sotrovimab, and VIR-7832 which is derived from sotrovimab. Moreover, COV2-2131+2196 performed almost similarly (see Fig. 6). Regrettably, only one of the three is authorized for emergency use- sotrovimab. Most important, the reason both sotrovimab, and VIR-7832 worked so well in this study is because they’re engineered to target conserved epitopes on omicron. In other words, epitopes are landmarks on a virus that don’t change from variant to variant. The most important data can be found in 2 graphs below (FIG. 5 A+B & FIG. 6) as they are the most comprehensive and measured current vaccine antibody, monoclonal antibody, and naturally acquired antibody protection against 1.)omicron, 2.) wildtype, VSV pseudoviruses carrying wild-type D614, and 3.) naturally acquired antibodies from previous infection. If you look at figure A, it shows the current protection of neutralizing antibodies from vaccinated and unvaccinated (convalescent) individuals. Overall, that data shows that protection is largely reduced from naturally acquired antibodies and monoclonal antibodies as the virus has mutated, that evidenced by the graph immediately below. Finally, figure 7 shows low IC50 values (purple bars) which indicate the potency of sotrovimab and VIR-7832. As the bars are smaller, less drug is needed to exert an effect compared to other monoclonal antibodies on the graph. That means sotrovimab and VIR-7832 monoclonal antibodies are still highly effective against the variant.
📸 FIG. 5 A+B
📸 FIG. 6
📸 FIG. 7
🤔 WHAT DOES ALL THAT DATA REALLY TELL US?
It seems that newer preprints, and even the drug companies themselves are suggesting the same thing. That being, there’s a strong correlation between omicron and reduced antibody efficiency. Said another way, it appears omicron has reduced the efficacy of most key monoclonal antibodies, naturally acquired antibodies, and vaccine induced antibodies. That means, public health officials need to consider utilizing the tools they have at their disposal like Pfizers antiviral pill Paxlovid (EUA approved 12/22/21), fluvoxamine (an SSRI/antidepressant already on the market), and even sotrovimab which seems to be the only monoclonal antibody working well anymore. An important fact, both Paxlovid and fluvoxamine in randomised control trials reduced hospitalization and death by 88% when averaged. So, what does all this mean for you anyways?
👪🏼What this means for you and your family
Primarily, there’s good and bad to take from this. So then it is true, one should evaluate both the positive and negative. Be that as it may, both the good and bad will be explored below.
Number one, the bad. The most detrimental element of all this new data is that outpatient treatments are not working well. That evidenced by omicron overpowering most monoclonal antibody treatments during lab experimentation. That is bad because currently few tools exist to combat SARS-CoV-2. So, losing the monoclonals sets everyone back in the fight against COVID for now. Of course monoclonals could be re-coded to work better, but regardless, that takes a lot of time. Furthermore, monoclonal antibodies have been in short supply lately. Even so, local health official announced recently they would be rationing sotrovimab, so don’t expect to see the only proficient monoclonal at your doctors office anytime soon if you catch COVID-19.
Number two, the good. The deficiency in COVID-19 treatments could hasten drug manufactures to develop new products. That wouldn’t be out of bounds as the cabinets are near bare. Intriguingly, the deficiency could spark inspiration and drive the market. Historically, there has been a strong proclivity for drug manufacturers to turn a profit when there’s a need, so it wouldn’t be surprising if that comes down the pike soon. The hope is that ingenuity and innovation do not come at an enormous cost in the middle of a pandemic. Next, all of this could create a push to repurpose old drugs. For instance, it’s already been seen with fluvoxamine, a cheap antidepressant drug (watch my video on this by clicking here). Not surprising, a cascade of randomised- controlled trails may begin popping up testing older drugs with excellent safety profiles. Time will tell.
Considering all salient facts, monoclonal antibody efficacy is waning. That evidenced by superbly low neutralizing power as omicron’s 15 receptor binding domain mutations get the best of current monoclonal antibodies, vaccine induced antibodies, and antibodies from natural infection. Regardless, we still need more data. Yet historically, the evidence shows us that when viruses become more contagious, they simultaneously become less deadly. As omicron is now highly transmissible, do you feel is it burning itself out and becoming less virulent?
https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern
https://covariants.org/variants/21K.Omicron
https://www.signaturescience.com/press/implications-of-the-mutations-in-the-spike-protein-of-the-omicron-variant-of-concern-voc-of-sars-cov-2/
https://www.ft.com/content/42c5ff3d-e676-4076-9b9f-7243a00cba5e
https://www.forbes.com/sites/williamhaseltine/2021/12/08/omicron-the-sum-of-all-fears/?sh=73c8640a5b51
https://www.sciencedirect.com/science/article/pii/S0966842X20303243
https://www.nature.com/articles/s41577-021-00542-x
https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/anti-sars-cov-2-monoclonal-antibodies/
https://www.nature.com/articles/s41598-021-99827-3
LETS CONNECT:











Omicron, like the other variants, is a nothing burger, PROVIDED you take prophalactic treatment and act correctly rarly on when you become ill. Once you're healthy again you scratch covid off your list of concerns. Stop the fearmongering.